‘A messy ball of wool’: the lived experience of obesity study
“Learnings from the study translate into direct insights for clinicians.”
Dr John Mercer
‘A messy ball of wool’ – a qualitive study of the dimensions of the lived experience of obesity
Obesity has a significant impact on individuals, communities and our broader health system, with an estimated two in three (67%) Australians aged over 18 estimated to be overweight or obese.
In Tasmania, about a third of the adult population is believed to be obese. However, the issue is a growing complex and multifaceted phenomenon which overlaps physiological, psychological and dietetic domains.
There is no easy fix.
Obesity is now recognised as a Chronic Health Condition in its own right, and significantly, a condition which exacerbates other health conditions. For decades, health professionals have been grappling with the best ways to treat and prevent the chronic condition, with the topic of obesity subject to extensive quantitative analysis.
While the outcomes from obesity interventions are usually measured in quantifiable terms – such as Body Mass Index – researchers are now starting to rethink their approach to obesity by focusing less on the medicine, and more on the person and their lived experience.
As part of a collaborative Tasmanian Health Service/University of Tasmania research team, last month Tasmanian researcher and Chronic Condition Psychologist Dr John Mercer presented the findings of new research aimed at rethinking the approach to obesity, at the Tasmanian Allied Health Symposium.
‘A qualitive study of the dimensions of the lived experience of obesity’ explored the social, psychological, and systematic factors preventing people with obesity from engaging with weight-loss interventions, while helping to formulate a response framework for clinicians.
Last month the paper was also included as one of 38 publications (from an original 12,388 screened) in a systematic review and qualitive synthesis on the lived experience of obesity.
Dr Mercer said understanding the lived experience of overweight and obese people, along with the self-perceived barriers for accessing and engaging in interventions, was imperative to forming a systematic response to the complex problem.
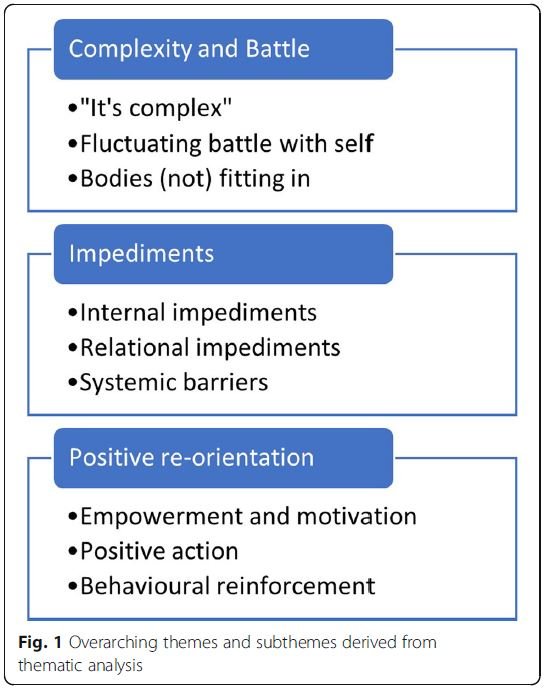
Based on the insights gained through focus groups and interviews with 26 participants all with a lived experience of being overweight or obese, the study identified three overarching themes: complexity and battle; impediments; and positive re-orientation – comprised of complex subthemes such as ‘failure’ and ‘control’.
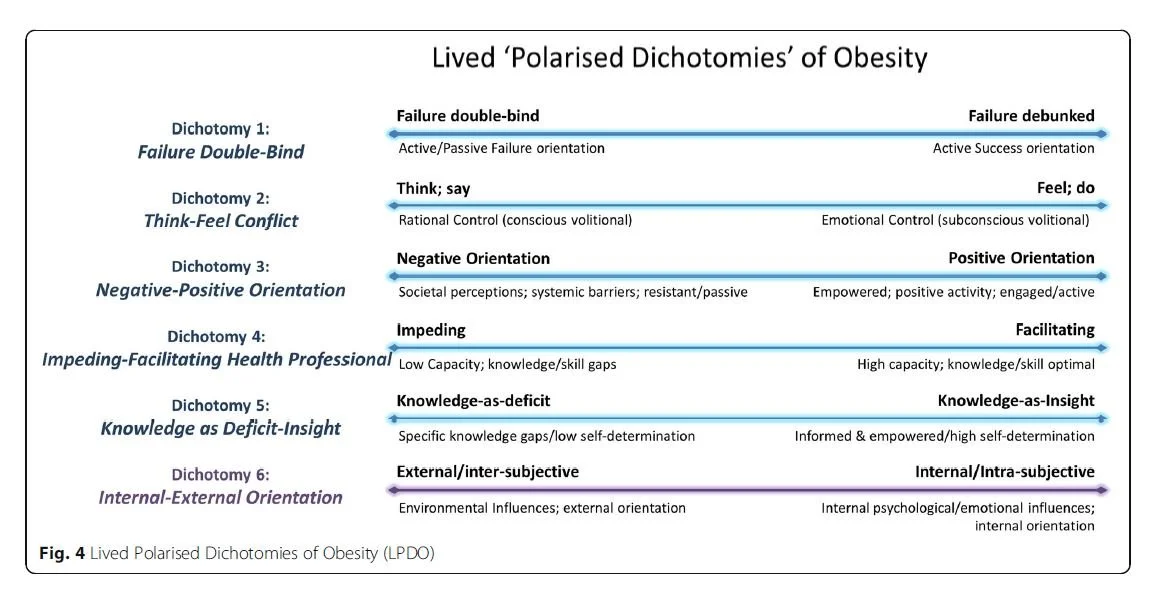
One participant described living with obesity as a “messy ball of wool”, with researchers suggesting the condition manifests as constraints and challenges across six “polarised dichotomies” – each active in the lived experience of the condition. The study found that each dichotomy had direct implications on a person’s ability to seek help for their condition.
The qualitative evidence suggests that if these dichotomies can be better understood and applied by practitioners, it will allow them to untangle each “messy ball of wool”, each complex and unique experience of living with obesity.
This includes the development of innovative, effective clinical practice interventions that individuals living with obesity want, need and will feel able to access.
First published late last year insights from the study have since been used to refine Dr Mercer’s latest research project, aimed at improving the outcomes of bariatric surgery patients.
Funded by the Clifford Craig Foundation, for more than a decade Dr Mercer has been collaborating with colleagues at the UTAS Clinical School in the area of obesity intervention, including assessing and working with pre and post bariatric surgery patients.
Here’s what he had to say on:
1 The need to rethink the approach to obesity, without perpetuating damaging stereotypes at a social level:
“At the reductionist level, it’s easy to understand obesity as a simple ‘energy’ equation: more energy in than out = energy stored. But that doesn’t account for complex human factors such as food choice, eating behaviour, and the motivations which underlie them. While at the biological level, excess calories equals weight, at more human levels, food choices (dietetic), behaviour and motivations (psychological) equal weight. It’s imperative then, that systemically, we reconceptualise obesity in ways that accommodate the biological, dietetic and psychological aspects of weight problems and interventions. “
2. The medicalisation of obesity over the years and the impact this has had:
“In developing the most accessible interventions and services possible, it’s important we recognise that obesity is a profoundly quantified health condition, and appreciate what this quantification can mean for the individual. Whether in kilos, BMI or centimetres, the quantification of a person can be experienced as dehumanising and alienating, reinforcing loaded emotions and compounding social stigma, and making it extremely difficult to approach a service or engage in an intervention.”
3. What this study will lead to:
“This qualitative study has done precisely what qualitative studies are supposed to do – explore the complexity of a phenomenon in ways that identify key questions for further quantitative investigation. As well as informing service system design at the local level, learnings from this project have identified key questions for subsequent research, investigating which factors predict the best outcomes from Bariatric Surgery. Perhaps as important though, learnings from the study translate into direct insights for clinicians, into the complexity of obesity as a lived experience. Ultimately, this means clinicians can respond in more sensitive, compassionate and effective ways.”